Turning 50 is a big milestone for many reasons! It’s a time when you might start thinking more seriously about your health, and one topic that often comes up for men is prostate cancer screening. You might have heard different things from friends, family, or even online, which can be confusing. Should you get screened? What does it even mean?
This article is here to clear up the confusion and give you the straightforward facts about prostate cancer screening when you hit the big 5-0. We’ll look at what prostate cancer is, how screening works, and why it’s not always a simple “yes” or “no” decision. Our goal is to help you understand your options so you can have a good talk with your doctor and make the best choice for your health.
Key Takeaways
- Prostate cancer screening at 50 is a personal choice. It's not a one-size-fits-all answer, and you should discuss it thoroughly with your doctor.
- The main screening tool is the PSA blood test, which measures a protein called Prostate-Specific Antigen. Higher levels can suggest a problem but don't always mean cancer.
- Screening has both benefits and risks. It can help find aggressive cancers early, but it can also lead to overdiagnosis and treatments with side effects for slow-growing cancers that might never have caused harm.
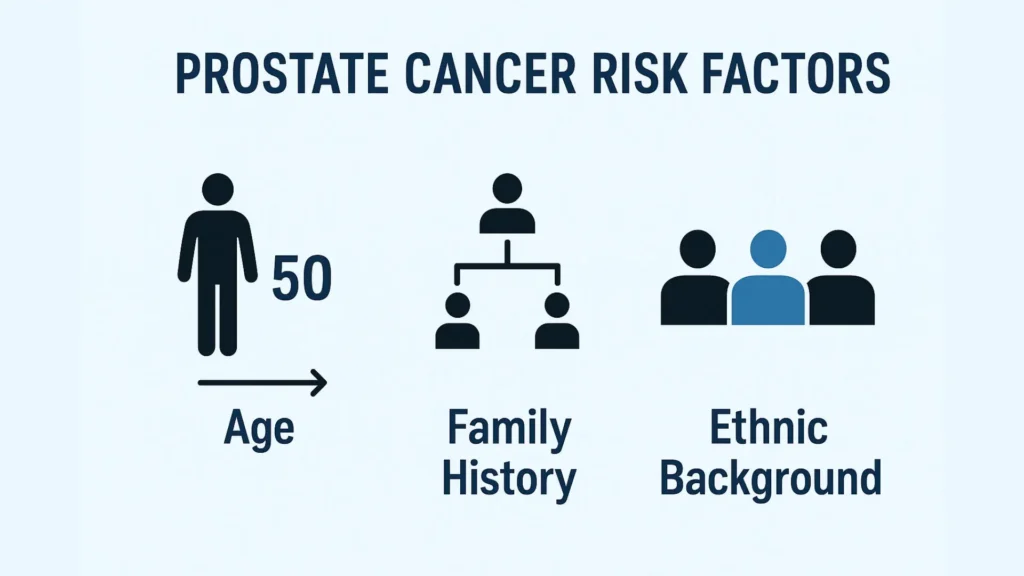
- Your risk factors matter. Age, family history, and ethnic background (especially African American men) play a big role in deciding when and if to start screening.
- Shared decision-making is key. You and your doctor should weigh your personal health, preferences, and risks together to decide if and when to begin prostate cancer screening.
Understanding Prostate Cancer Screening: What You Need to Know
Before we dive into screening, let's get a basic understanding of what prostate cancer is. Knowing the basics will help you make more sense of why screening is such an important, yet sometimes complicated, topic.
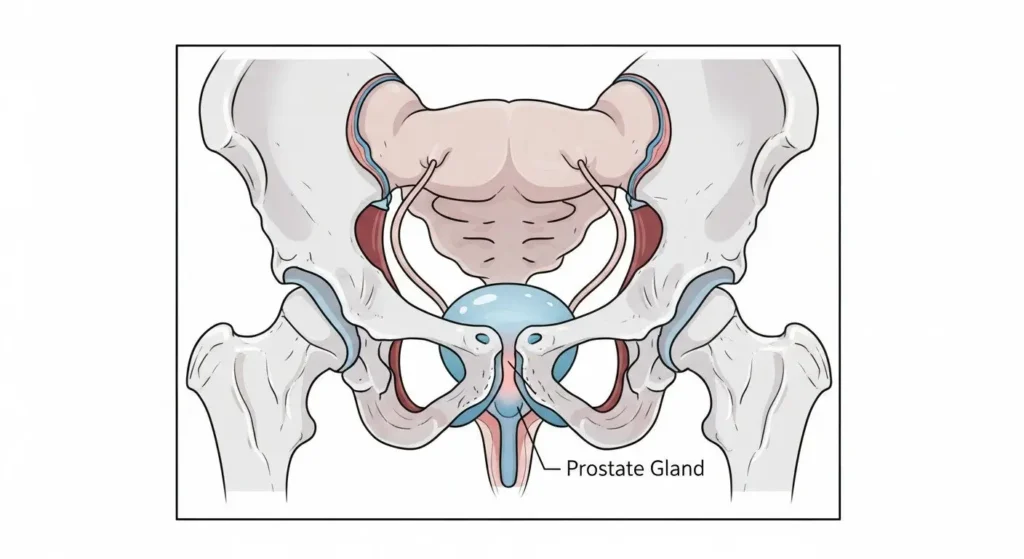
What is the Prostate?
The prostate is a small gland, about the size of a walnut, that is part of the male reproductive system. It sits just below the bladder and in front of the rectum. Its main job is to produce a fluid that helps carry sperm. The urethra, the tube that carries urine and semen out of the body, passes right through the prostate.
As men get older, the prostate can grow larger. This is a common condition called Benign Prostatic Hyperplasia (BPH), which is not cancer. However, this growth can sometimes cause problems with urination.
What is Prostate Cancer?
Prostate cancer happens when cells in the prostate gland grow out of control. Most prostate cancers grow slowly and stay within the prostate gland, often causing no serious problems for many years. Some types, however, can be aggressive, meaning they grow quickly and can spread to other parts of the body.
Prostate cancer is one of the most common cancers among men. In the United States, about 1 in 8 men will be diagnosed with prostate cancer during their lifetime. It's more common as men get older, with the average age of diagnosis being around 66. This is why discussions about screening often start around age 50.
“Knowledge is power, especially when it comes to your health. Understanding your prostate is the first step.”
Why is Early Prostate Cancer Screening Important?
For aggressive prostate cancers, finding them early, before they spread, can mean better treatment options and a higher chance of a full recovery. When cancer is limited to the prostate, treatments are often more effective. However, as we'll discuss, not all prostate cancers need immediate treatment, and some might never cause harm. This balance is what makes the screening decision complex.
The PSA Test: A Closer Look at Prostate Cancer Screening Tool
When doctors talk about prostate cancer screening, they are usually talking about two main tests: the Prostate-Specific Antigen (PSA) blood test and, less commonly, the Digital Rectal Exam (DRE).
What is PSA?
PSA stands for Prostate-Specific Antigen. It's a protein made by both normal and cancerous cells in the prostate gland. A PSA test measures the level of this protein in your blood.
- How it works: A small sample of your blood is taken, usually from your arm, and sent to a lab.
- What it shows: Higher levels of PSA in the blood can suggest a problem with the prostate. This could be cancer, but it could also be other non-cancerous conditions like an enlarged prostate (BPH) or an infection (prostatitis).
What Do the Numbers Mean?
There isn't a single “normal” PSA level that applies to everyone. Generally, a PSA level below 4.0 ng/mL is considered low, but even levels below 4.0 can sometimes be linked to prostate cancer. Regular prostate cancer screening is important, especially as men get older and their PSA levels naturally tend to rise.
Here's a general guide, but remember, your doctor will interpret your results based on many factors:
| PSA Level (ng/mL) | What it Might Mean |
|---|---|
| Below 2.5 | Generally considered low risk for cancer, but still not a guarantee. |
| 2.5 – 4.0 | Borderline. Your doctor might suggest monitoring or further tests, especially if you have other risk factors. |
| 4.0 – 10.0 | Moderately elevated. This is often where doctors start considering a biopsy, but it could still be a non-cancerous issue. |
| Above 10.0 | High. This level raises more concern for prostate cancer, and further investigation (like a biopsy) is usually recommended. |
Important Note: A high PSA level does not automatically mean you have prostate cancer. Many men with high PSA levels do not have cancer, and some men with prostate cancer have low PSA levels. That's why the PSA test is an essential part of prostate cancer screening, serving as a preliminary tool rather than a definitive diagnostic measure.
The Digital Rectal Exam (DRE)
The DRE is another screening tool where a doctor gently inserts a gloved, lubricated finger into the rectum to feel the prostate gland. They check for any bumps, hard areas, or unusual changes in size or shape that might suggest cancer.
While the DRE can sometimes detect cancer that a PSA test might miss, it's often considered less effective than the PSA test for initial screening. Many doctors use both tests together, or rely primarily on PSA and then use DRE if PSA is elevated or other concerns arise.
The Great Debate: Prostate Cancer Screening at 50
This is where things get interesting! For many years, there has been a big discussion among doctors and health organizations about whether all men should undergo prostate cancer screening, especially starting at age 50. There are strong arguments on both sides.
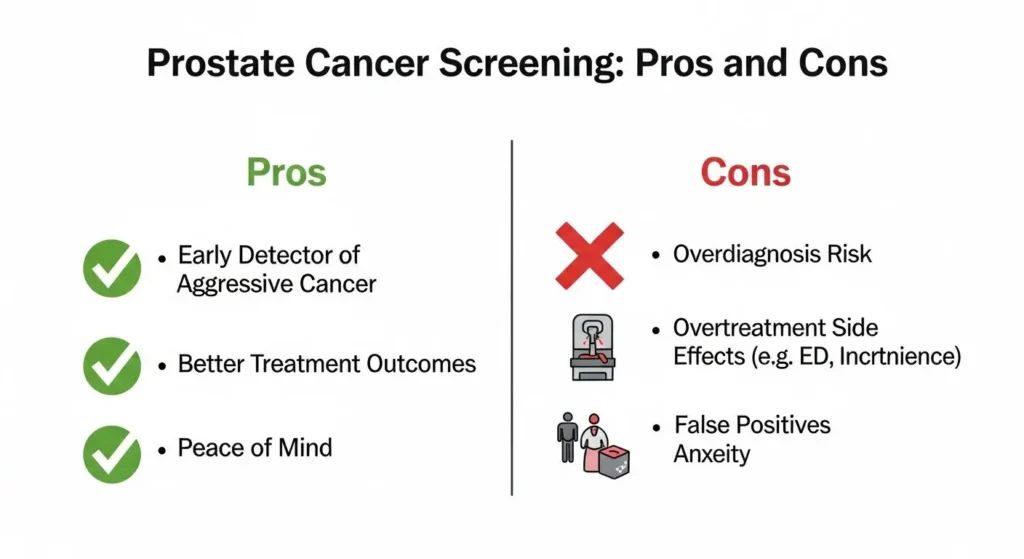
Arguments For Screening (The “Pros” )
- Early Detection of Aggressive Cancer: For men with fast-growing, aggressive prostate cancer, finding it early through screening can be a lifesaver. It allows for treatment when the cancer is still contained, leading to a better chance of cure.
- Peace of Mind: For some men, knowing their PSA level is normal brings peace of mind.
- Informed Choices: Screening can give men and their doctors important information to make decisions about their health.
Arguments Against Screening (The “Cons” )
- Overdiagnosis: This is a major concern. Many prostate cancers grow so slowly that they would never cause problems or shorten a man's life. Screening can find these “harmless” cancers.
- Overtreatment: When these slow-growing cancers are found, men often choose to treat them with surgery, radiation, or other methods. These treatments can have serious side effects, including:
- Erectile dysfunction: Difficulty getting or keeping an erection.
- Urinary incontinence: Leaking urine.
- Bowel problems: Issues with digestion or bowel control. These side effects can significantly impact a man's quality of life, even if the cancer itself was not life-threatening.
- False Positives: A high PSA level can lead to more tests, like biopsies, even when no cancer is present. Biopsies carry their own risks, such as pain, bleeding, and infection.
- Anxiety: The process of screening, waiting for results, and potentially undergoing further tests can cause significant stress and anxiety.
Medical Organizations Weigh In
Different major health organizations have slightly different recommendations, which adds to the confusion!
- American Cancer Society (ACS): Suggests men should have an informed discussion with their doctor starting at age 50 about the pros and cons of prostate cancer screening. For men at higher risk (African American men or those with a close relative who had prostate cancer before age 65), discussions should start earlier, around 40 or 45.
- U.S. Preventive Services Task Force (USPSTF): Recommends that men aged 55 to 69 should make an individual decision about screening, after talking with their doctor about the potential benefits and harms. For men 70 and older, they recommend against screening.
- American Urological Association (AUA): Recommends shared decision-making for men aged 55 to 69. They suggest that screening may be considered for men aged 40 to 54 who are at higher risk.
The key takeaway from all these guidelines is shared decision-making. This means you and your doctor talk it over, considering your unique situation, and decide together what's best for you.
Who Should Consider Screening? Your Risk Factors
While age 50 is a common starting point for discussions, some men might need to consider screening earlier due to certain risk factors.
Age
The risk of prostate cancer goes up with age. It's rare in men under 40, but the chance of getting it increases significantly after age 50. That's why 50 is often the benchmark age for these discussions.
Family History
If your father or brother had prostate cancer, especially if they were diagnosed before age 65, your risk is higher. The more close relatives you have with prostate cancer, and the younger they were when diagnosed, the greater your risk.
Ethnic Background
African American men have a higher risk of developing prostate cancer compared to other races. They are also more likely to get it at a younger age and to have more aggressive forms of the disease. Because of this, screening discussions might start earlier for African American men, often around age 40 or 45.
Other Factors
While less direct, some lifestyle factors might play a role in prostate health:
- Diet: A diet high in red meat and dairy, and low in fruits and vegetables, might increase risk.
- Obesity: Being overweight or obese may increase the risk of more aggressive prostate cancer.
If you're looking to support your prostate health through diet or supplements, you might find useful information in resources like the most effective prostate supplements reviewed for 2025. For a broader guide, consider understanding and choosing prostate supplements.
The Screening Process: What to Expect
If you decide with your doctor to move forward with prostate cancer screening, here's a general idea of what to expect.
1. Initial Discussion with Your Doctor
This is the most important first step. Your doctor will talk to you about your personal risk factors, your overall health, and your feelings about the potential benefits and harms of screening. They should explain:
- What the PSA test involves.
- What different PSA results might mean.
- The possibility of false positives and false negatives.
- The risks and benefits of further tests (like biopsies) and treatments.
2. The PSA Blood Test
If you decide to proceed, a blood sample will be taken. It's a quick and simple procedure, much like any other blood test.
3. Digital Rectal Exam (DRE) (Optional)
Your doctor may also perform a DRE during your physical exam. This can sometimes provide additional information alongside the PSA test.
What Happens if Your Results Are Abnormal?
If your PSA level is elevated or your DRE is abnormal, it doesn't automatically mean you have cancer. It means your doctor will want to investigate further.
- Repeat PSA Test: Sometimes, a PSA test is repeated after a few weeks to see if the level has changed.
- Further Blood Tests: Other blood tests, like a “free PSA” test, might be used to help determine the likelihood of cancer.
- MRI Scan: An MRI of the prostate can help doctors see suspicious areas more clearly and guide further steps.
- Prostate Biopsy: This is the only way to definitively diagnose prostate cancer. During a biopsy, tiny tissue samples are taken from the prostate with a needle and examined under a microscope. This is usually done with local anesthesia.
If you're facing prostate problems and exploring solutions, you might be interested in how Prostavive tackles prostate problems head-on. For a natural approach, consider reading about Prostavive as a natural solution for prostate health.
Interpreting Your Results and Next Steps
Getting results can be stressful, but understanding them helps.
Normal PSA or DRE
If your PSA is low and your DRE is normal, your doctor will likely recommend continuing with routine check-ups and follow-up discussions about future screening, depending on your age and risk factors.
Elevated PSA or Abnormal DRE (But No Cancer Diagnosed)
As mentioned, an elevated PSA doesn't always mean cancer. Your doctor will look at your PSA level, how much it has changed over time (PSA velocity), your age, risk factors, and DRE results to decide on the next steps. This could involve:
- Watchful Waiting/Active Surveillance: Simply monitoring your PSA over time.
- Further Tests: More specialized blood tests, urine tests, or an MRI.
- Biopsy: To check for cancer cells.
Diagnosed with Prostate Cancer
If a biopsy confirms prostate cancer, the next steps depend on several factors:
- Grade of Cancer (Gleason Score): How aggressive the cancer cells look under a microscope.
- Stage of Cancer: Whether the cancer is confined to the prostate or has spread.
- Your Age and Overall Health: Your life expectancy and other health conditions.
- Your Preferences: Your personal values regarding treatment side effects.
Based on these, treatment options can range from:
- Active Surveillance: For slow-growing, low-risk cancers, doctors might recommend closely monitoring the cancer with regular PSA tests and biopsies, rather than immediate treatment. This helps avoid overtreatment side effects.
- Surgery: Removing the prostate gland (radical prostatectomy).
- Radiation Therapy: Using high-energy rays to kill cancer cells.
- Other Treatments: Hormone therapy, chemotherapy, or newer targeted therapies for more advanced cases.
Making an Informed Decision: Your Role
Ultimately, the decision to undergo prostate cancer screening at 50 is yours, in partnership with your doctor. This is called “shared decision-making,” and it's crucial for a condition like prostate cancer where the benefits and harms of screening and treatment are finely balanced.
Here’s how you can prepare for this important discussion:
- Know Your Family History: Gather information about any close relatives (father, brothers) who had prostate cancer, and at what age they were diagnosed.
- Understand Your Ethnic Background: If you are an African American man, be aware of your increased risk.
- Think About Your Values: How do you feel about potential side effects of treatment versus the risk of missing a serious cancer? Are you comfortable with the idea of active surveillance if a low-risk cancer is found?
- Write Down Questions: Don't be afraid to ask your doctor anything that's on your mind.
Here are some questions you might ask your doctor:
- “Given my age and health, what are my personal risks for prostate cancer?”
- “What are the benefits of screening for me?”
- “What are the harms or risks of screening for me?”
- “If my PSA is elevated, what are the next steps, and what are the risks of those steps?”
- “If I am diagnosed with prostate cancer, what are my treatment options, and what are the side effects?”
- “What is ‘active surveillance,' and could that be an option for me?”
- “How often should I be screened, if we decide to go ahead?”
“Your health, your choice. Make it an informed one.”
Beyond Screening: Maintaining Prostate Health
While screening focuses on detecting cancer, maintaining overall prostate health is also important. A healthy lifestyle can play a role in reducing your risk for many health issues, including potentially some prostate problems.
Healthy Lifestyle Choices
- Balanced Diet: Eat plenty of fruits, vegetables, and whole grains. Limit red and processed meats, and high-fat dairy products. Some studies suggest that a diet rich in lycopene (found in tomatoes), selenium, and vitamin E might be beneficial, though more research is needed.
- Regular Exercise: Staying physically active helps maintain a healthy weight and improves overall health.
- Maintain a Healthy Weight: Obesity is linked to a higher risk of aggressive prostate cancer. If you're looking into managing your weight, you might find information on Liv Pure reviews and what to expect helpful for overall wellness.
- Limit Alcohol: Moderate alcohol consumption is generally fine, but heavy drinking can affect overall health.
- Don't Smoke: Smoking is a known risk factor for many cancers, including potentially more aggressive prostate cancer.
Prostate Supplements
Many men explore supplements to support prostate health. While supplements are not a cure or a replacement for medical advice, some ingredients are often studied for their potential benefits. These might include:
- Saw Palmetto
- Beta-sitosterol
- Pygeum
- Rye Grass Pollen Extract
- Zinc
Always talk to your doctor before starting any new supplements, as they can interact with medications or have their own side effects. For a deeper dive into options, check out our guide on Prostavive: the natural solution for prostate health.
Conclusion
Deciding whether to begin prostate cancer screening at age 50 is a significant personal health decision. There's no single right answer for everyone, and it's crucial to weigh the potential benefits of early detection against the risks of overdiagnosis and overtreatment.
The most important step you can take is to have an open and honest conversation with your doctor. Discuss your personal risk factors, your health history, and your values. Together, you can make an informed choice that aligns with your health goals and gives you the best path forward. Remember, staying informed and proactive about your health is always a good thing!